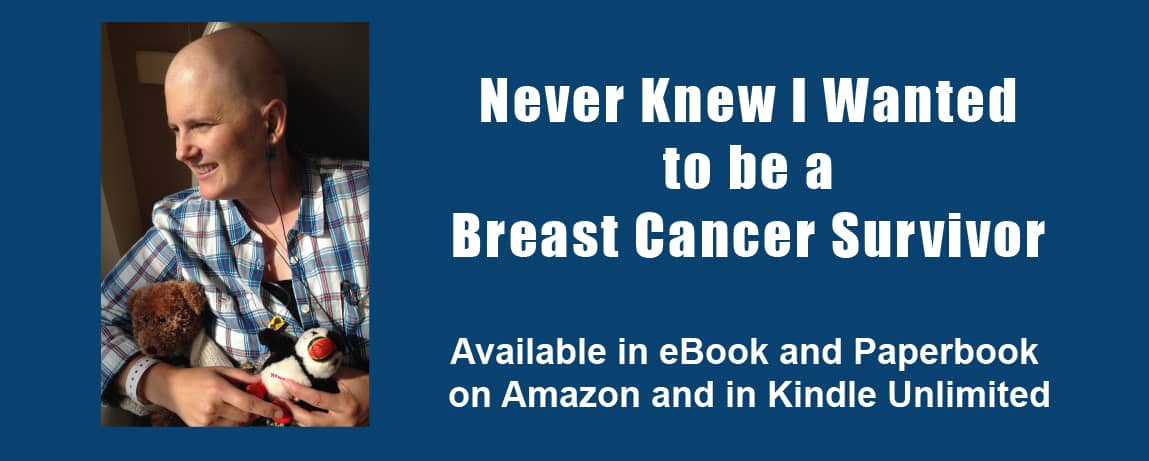
This post is a continuation on my discussion about Patient Health Literacy. The narrative that resulted from this study has been published on Amazon. See my Memoir page. The original source that I used for my study can be found at https://bcbecky.com.
In reviewing the posts categorized as Navigating the healthcare system, I constructed the following themes: (1) learning processes, (2) taking control, (3) dealing with insurance, and (4) waiting. The theme learning processes applies to posts where I describe the different interactions I’m having with healthcare providers. The theme taking control applies to posts where I voice my need to empower myself or others by exerting some form of control over a situation. The theme dealing with insurance applies to posts where I write about issues insurance coverage of medication and treatments. The theme waiting applies to posts where I write about issues with waiting for various test results or treatments. I discuss each of these themes in more detail in the in the following sections.
Learning Processes
In the beginning I had no understanding of how the medical system worked with respect to cancer treatment. My understanding came only from what I saw on television and from an acquaintance that I sailed with 15 years ago who happened to be a medical oncologist. From that, I knew that there were different types of oncologist, but I did not understand that breast cancer treatment typically begins with surgery. Throughout the blog, I explore and share my interactions with the medical system, as I learn to negotiate it.
In Canada, I likely would not have had much choice in where I received treatment. I also would not have thought that a I had any choice in surgeon or oncologist. I would go to who I was referred to. In the US, and specifically in the area where I live, there are multiple providers. In some ways insurance affects where you get treatment, but I had really good insurance that allowed me the option of choosing. After hearing the words ‘you have cancer’ I felt an immediate sense of lack of control. The ability to choose a healthcare provider, although stressful and a completely new process for me, was also a way to exert some control over the situation.
As all the processes were new to me, I explained them in detail as they occurred. For example, in A long day (June 19, 2014), I explain the process of the appointment with the surgeon as well as the “whirs, honks, and other sounds” associated with my first experience with magnetic resonance imaging (MRI). I continue with the description of processes on my first day of chemotherapy, where I also include images that provide visual documentation of the process (First day of chemo, July 7, 2014). Further, in This too shall pass (July 16, 2014), I describe how:

In addition to describing the medical process, I also described what I learned about the process of gathering information from my care team. In I had to give myself permission to nap (July 9, 2014), I outline what I learned about how nurses and physicians provide different levels of information:
My analysis also shows that, in addition to describing the processes as I recalled them, I also wrote about my observations regarding medical education from the interpersonal perspective:
Finally, when I was hospitalized after surgery, I described my experience with hospital processes, specifically how a private room meant that my husband could stay the night with me, and the quality and process of getting food: “One thing that impressed me about the university hospital is that they use a room service model for food. The menu is quite good, and so far, the food has been good. The food is locally sourced where possible, and there are organic options” (An update from the hospital, November 20, 2014).
Taking Control
From the beginning I tried to take control by booking appointments for a second opinion from the university healthcare system. Here I was immediately frustrated at an inability to get an appointment without a confirmed pathology. Fortunately, they did guarantee me an appointment when the pathology results were confirmed (The speed of things, June 15, 2014). After getting an appointment, the act itself of seeking a second opinion and making a choice as to where to get healthcare were ways that I could take control (Double-mastectomy and chemo, June 19, 2014).
When I began to experience some odd side effects, specifically blisters on my hands, that were not resolving, we made the decision to go to the emergency room. This was in part so that we could experience the process of the emergency room at a time when we were not overly stressed – that is, “while I was happily ambulatory and not ‘really sick’, just in case I needed the services at a later time” (Not without incident, July 13, 2014). Further, in Engaged patient in a hospital gown? (September 27, 2014), I describe the process of a typical doctors’ appointment – and how I take as much control as I can during those appointments, in this case by wearing a hoody over the hospital gown.
Dealing with Insurance
The role of insurance in the treatment for breast cancer both surprised and outraged me. I was surprised when one of the first things the surgeon told me, after telling me he recommended a double mastectomy, was the ‘good news’ that insurance was required to pay for reconstruction (How do you prepare to lose a body part?, June 15, 2014). I was surprised when the oncologist mentioned that “it also takes about a week to get approvals from the insurance company” (Caution – this one talks a bit about death, June 21, 2014) before I could start chemotherapy.
We ran into issues with insurance and treatment after my first day of chemotherapy, which required the white blood cell booster Neulasta to be administered the following day. Insurance changed the way in which it was to be delivered (Pains with the American System, July 7, 2014). Finally, with a slightly more nuanced understanding of the way insurance impacts healthcare in the United States, I write a response to a New York Times article expressing my concern “that research stated like this gives insurance companies a reason not to pay for the surgery, when it may be in the best interest of the individual” (Bilateral mastectomies, July 28, 2014).
Waiting
Waiting was something that I ran into from the very beginning. First it was waiting for the pathology results, as I could not make an appointment at the university cancer center without confirmed pathology (The speed of things, June 16, 2013). When we were deciding on where to get treatment, we knew that we would be spending more time waiting at the university cancer center. We took waiting into consideration when making our decision, specifically I write:
As I went through treatment, there were many occasions where I describe what I felt to be excessive wait times. For example, “It turned into a long day. We had a delay seeing the nurse practitioner to get sign off on chemo – unfortunately that turned into a three-hour delay. Then we had a delay on the saline drip for rehydration, which added another additional hour” (AC Cycle 4, August 19, 2014).
As we became more familiar with processes, we became more efficient with our time, developing strategies to reduce the amount of time we spent waiting. When I became more confident in myself as a patient advocate, I learned to identify problems in the system and articulate them to management in hopes of resolving the issue. For example, in Learning to assert myself, (October 29, 2014), I write:
Summary
Nursing research shows that supporting breast cancer patients with navigating the healthcare system can improve many aspects of the care that patients receive (Robinson-White, Conroy, Slavish, & Rosenzweig, 2010). My analysis of the category Navigating the healthcare system shows that I had regular interactions with the healthcare system, and there were spikes in my interactions associated with receiving pathology results, starting chemotherapy, exploring surgery options, and surgery itself. Under the category Navigating the healthcare system, I constructed the following four themes: (1) learning processes, (2) taking control, (3) dealing with insurance, and (4) waiting. As I learned the processes associated with receiving cancer care, I wrote about them. When I was able to, I sought ways that I could take control over my interactions with the healthcare system. Unfortunately, there were two areas of challenge with my experience with the healthcare system, dealing with insurance and what felt like unnecessary waiting.
Each person experiences breast cancer differently. This difference is in part related to the variable nature of the disease, but also the different healthcare systems where the patient is seeking treatment. The nursing profession has attempted to address this complexity with the creation of formal nurse navigators that help guide cancer patients through the healthcare system (Case, 2011). Unfortunately, not all healthcare systems have nurse navigators. In addition, the nurse navigators are often not fellow breast cancer survivors. This means that they cannot fully appreciate what it means to live with the illnesses associated with breast cancer and its treatments. The nurses are also insiders within the system, with knowledge and privileges that patients do not have. This can lead to a gap in what information the patient needs. Patients experiencing critical or chronic illness have a need to learn how to navigate the healthcare system from a patient perspective.

Leave a Reply