I love to take selfies when I hike. I’d like to share my year in selfies … some of you might recognize yourself in the pictures 🙂
Category: Navigating the new me
-

Neuropathy update
It has occurred to me that it has been a long time since I’ve talked about my chemotherapy induced peripheral neuropathy. At about this time last year I saw a pain doctor. Just in passing he mentioned the option of a 24-hour time released gabapentin (known as Horizant). It often isn’t mentioned because it isn’t on most insurance formularies (meaning it costs patients more). One big reason to chose it is that it reduces pill fatigue. One point that insurance companies and doctors seem to miss that is that it works a lot better. It is unfortunate that the efficacy of a medication isn’t taken into account because of insurance companies, and it really annoys me that insurance companies don’t take into account the efficacy of the medication. It is one of the things that angers me the most about this healthcare system.
One of the biggest advantages to a time-released version of the medication is that it is always in your system. With the other gabapentin, I’d need to take 4-pills every 6-hours for it to be equivalent. That means waking up in the middle of the night. On gabapentin, my neuropathy was always worse first thing in the morning. That was, in part, because after 8-hours of sleep I no longer had gabapentin in my system. Gabapentin also makes some people drowsy. So taking it 4-times per day can be really disruptive. The horizant makes me drowsy, so I take it at dinner and it helps me sleep at night (a double win because hormone therapy mucks with sleep patterns).
For me, Horizant has been a miracle drug. I’m willing and able to pay the extra for it (it isn’t cheap). It means that when I wake up first thing in the morning, my feet don’t hurt. It also means that my feet don’t hurt when I get up after sitting. It used to be that the first 10 steps were filled with burning pain in my feet.
I’m noticing that my neuropathy is improving. I still go through phases where things burn, but then they are much less intense. I notice that I have much more feeling in my lower legs and feet. This makes getting IVs in the legs a lot more painful, but that is a worthwhile trade-off for improved neuropathy. It used to be that I would lose feeling in my feet after 20 minutes of hiking. Now I don’t even notice my neuropathy until around the 90-minute mark. And even then, what I’m noticing is not nearly as bad as it used to be. So, I’m happy to report that my neuropathy is improving.
In January, I’ll talk to the pain doctors again. Anytime I mention going off of the Horizant, it is suggested that I stay on it. It is also used for other medical conditions that I have, like back pain from arthritis, reducing the side-effects of hormone therapy (e.g. making hot flashes less severe, treating restless leg syndrome), and treating post-surgery fantom pains. My healthcare team feels it is doing more for me than just treating my neuropathy.
And so, as this year is coming to a close, I’m happy to report that my neuropathy is doing much better. I’m finally starting to feel like I’m getting at least some of my health back. I’m hiking further than I ever used to – with a 10km (6-mile) hike not being out of the ordinary.
-

Patient Health Literacy
I posted this originally over on my academic blog: http://rjh.goingeast.ca. However, I think those who read this blog are in a better position to answer the question I’m asking at the bottom – so please bear with some of the academic language.
In Arthur Frank’s (1995) seminal book The Wounded Storyteller, he cautions “On rare occasions when I have taught this book, students’ biggest initial difficulty is to stop reframing everything ill people say into a question of how some health-care worker might respond.” (Location 115)
I often find myself falling into that trap. I find myself thinking about my research, and the focus on peer-to-peer patient learning, and yet seem to feel that the value in the research is in the change in how health-care workers respond. Really, my focus should be a change in how my work can help patients and caregivers find agency within the healthcare system.
This idea of value of knowledge (or value of literacy) is something that Brian Street talks about in Social Literacies: The Schooling of literacy. I talked a little about it in my post on critical digital health literacy. In the chapter I’m reading now, Street (1995) talks about how the definition of what literacy is (the value proposition) is defined by the dominant culture. When we talk of a critical literacy, we are turning that around and looking at it from the perspective of the non-dominant – perhaps those who are seen as not literate.
In the health literacy context, we see the definition of digital health literacy from the perspective of healthcare systems – “the ability to seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem” (Norman & Skinner, 2008, para. 6). To me, this definition feels like what health professional want patients to have, not what patients necessarily want or need. The health literacy definition is from the perspective of the dominant culture. It is also very solution oriented – as if there were only one solution to the “health problem”. The human body is complex. It is a complex system. There are many different ways in which to approach a health problem, and not all of those involve solutions.
Now if I look at it from my perspective as a patient, and not a healthcare professional, I can see literacies in a different light. If I look at what I consider important to be “health literate” from a patient perspective, I’d say:
- Understanding the disease well enough to explain it to both non-medical professionals and medical professionals (knowing that the language of the medical profession is not the same as the language used by the general population).
- Understanding the healthcare system well enough to get the care you are looking for. This in part means knowing who to ask which questions to, and knowing even what things are available to you as a patient. Understanding the hierarchies within the healthcare system helps to ensure you are asking the right people the right questions.
- Knowing where to go to get support from peers.
- Knowing how to identify individual experiences of disease experience versus generalized experiences. That is, developing an understanding of what aspects are typical and what aspects are unique to the individual experiencing the disease.
- Understanding the disease well enough to search for information on the internet, and discern appropriate sources of information (e.g. being able to identify snail oil).
My question to you is, as a patient, what you see as the important things YOU need to know in order to manage your personal health?
Feature image: By NASA/MSFC/David Higginbotham – NASA Image of the Day, Public Domain, Link
-

New hair day
I’m a little obsessed with my hair. Not in a need to be a fashionista kinda of way, just in a way in which my hair fell out, and the way in which it is recovering from the effects of chemotherapy.
Yesterday I got my first hair style in years (too many really). Even before cancer, I had pretty consistent hair style for about 3 years, and then with cancer I lost all my hair. So, it is a bit of a milestone to get a new haircut that wasn’t about trimming off the post-chemo frizz.
I have to say I’m really happy with the way it turned out. The stylist actually listened to me when I told him “I’m a wash and wear kind of gal”. I don’t even own a blow dryer or hair iron of any sort. So to have something that looks decent and doesn’t require a lot of maintenance is awesome.
I’m also not someone who typically wears make up. I never have been. But I noticed in all the video conferencing that I do that I don’t like how my face looks. I realized that something was not quite right. My eyebrows didn’t really recover from the chemo loss. I have eyebrows but not thick ones. This means that when I sweat, it drips into my eyes – which is exceedingly frustrating, but I also realized that in head shots, not having eyebrows makes my face look round and chubby. It took me quite a while to realize it was the lack of eyebrows that made me feel like I didn’t look right. And so, with that realization, I bought an eyebrow pencil/brush thing. I’ve started to fill in my eyebrows when I know I’m going to be online or going out to visit people (although not for hiking, as then I’d just get eyebrow make up in my eyes!
I find this new obsession with hair to be interesting. It isn’t just hair on my head, rather hair all over my body. When my arm hairs grew back they came up in every which direction. My original arm hair grew all one way. It felt tamed. Although no one other than me sees my arm hair (unless I show them), it still is something that is different. In some ways it is fascinating, in others it is just odd.
-
Does participation in the breast cancer blogosphere increase anxiety?
I just read an article about eHealth literacy and anxiety and it got me thinking. Actually I’ve been thinking about it a fair bit lately – since my last appointment with my breast surgeon. At that appointment, the nurse practitioner told me “you have been cured”. It is the first time that someone has used the word “cured” about my cancer. I also found myself wondering if it was appropriate. I wondering if “no evidence of disease” is a better term than “cured”. I’m pretty sure my medical record says “NED” rather than “cured”. At my 6 months follow up I made my surgeon say “no evidence of disease” out loud because I needed to hear those words. But this got me thinking. If I didn’t know as much about breast cancer and recurrence, would I feel better about being told I was cured? Would I believe it and would it allow me to move on with my life with less anxiety?
I found that being prepared for chemotherapy helped reduce my anxiety about it. I had read a lot, as had my husband. We had some sense of what I would be experiencing. I had mentors (that is the best word I can think of – peers who were ahead of me in the chemo process), who helped me feel more prepared for chemo. So, being health literate helped reduce my anxiety as I went through active treatment.
But now that active treatment is over, the health literacy isn’t helping me. I know too much about this disease. I know that because of my age I’m at increased risk for recurrence. The information that I have means that I cannot simply accept it when the nurse practitioner uses the word “cured”. I cannot believe it. It does not help me feel less anxious.
I’m left wondering if I would have had the same reaction post-treatment? Would I have found my self as anxious, if I wasn’t so aware. For me, being aware helped me advocate for myself during active treatment – but now it just makes me question. It makes it harder for me to trust my healthcare team. I find myself not believing when they tell me I’m OK. I’m doing fine. I’m cured.
It makes me wonder, does participation in the breast cancer blogosphere make me more anxious? Or is it participation in support groups that is causing an increase in my anxiety? Or is it just that I’m in that post treatment phase and anxiety is something that was going to happen to me anyways?
Feature image by NYPhotographic.com license CC BY-SA 3.0 NY
-

The difference a year makes
I’d like to be saying that this year I feel stronger and fitter than I did at this time last year. I’m not sure I can say that. But… I am definitely healthier.
This time last year I got my official diagnosis of celiac disease, lymphedema, and high blood pressure — pretty much all at the same time — October 28th. I remember that day quite clearly.
In the last month I’ve learned that I don’t have any signs of cancer, I got cleared for 1 year follow-ups with my breast surgeon, I’m showing no signs of the celiac anti-bodies (it took a year on gluten free diet for them to clear up), my blood pressure is under control, and I have no pre-clinical signs of lymphedema (which means, not only do I not have any visible swelling, I’m also clear on the impedance test that they do – so that is an every 3-month scan that I no longer need). In addition, I finally got to the surgery to clean the arthritis in my toe, and although it hurts, the pain is not nearly as bad as it was before the surgery!
Last year at this time I was exploring the idea of going back to my PhD. I was starting to feel ready. I’m now back at it, I’m teaching and working on my dissertation. I’m enjoying both, and wishing I had more time and a better ability to concentrate, but I’m making good progress.
These last two months have been difficult for me emotionally. I’ve been dealing with a lot of death – death of my father, and the death of a couple breast cancer friends.
So, although I feel like I should be celebrating. I feel a bit tired. I want to get back to exercising regularly, but my darn toe just isn’t cooperating. I’m hobbling a little and will hopefully be able to jump in the pool tomorrow, even if it is just for a short swim. Something is better than nothing.
Now I probably am healthier than this time last year. It was actually the year before that I last felt physically stronger. Last year the lymphedema slowed me down. I haven’t yet gotten back into regular cycling. I have since done a lot more swimming – where I now typically swim a mile. I have done a fair bit of hiking in the last year, regularly getting out to Alum Rock park for a 7km loop.
I feel a little like this is a rambling post, but I felt I needed to make it. I’m fighting the emotional blues while knowing that I should feel good about how much better I’m doing this year. It is hard for me to feel good about how I’m doing when a good friend is not sure yet if the new chemo will work – and she is out of alternatives. Things are on an upswing for me, let’s just hope it stays that way!
Feature image CC0 via Pixels.
-
I wish someone told me …
Lucinda: “I wish someone told me more about how my reconstructed breasts would look after surgery. I wish I knew that when I flexed my muscles my breasts would move sideways leaving a flat gap between them. It seem so unnatural. I wish someone told me that when I exercise they would move this way.
Lucinda: “I was at a conference last week and I learned that there is a name for this. It is called I was surprised to learn there is a name for this. It is called ‘window shading‘. It is common enough that they have given it a name, and yet no one told me.”
Surgeon: “When would you have wanted to be told?”
I was having a conversation with my friend Lucinda yesterday. We were talking about information overload, but also the desire to know more about the potential issues/complications with our reconstruction surgeries.
Having done neo-adjuvant chemotherapy, I had a lot of time to research my surgery. I learning a lot about possible side effects not from the literature, but rather from participating in online support groups (e.g. there is a DIEP flap Facebook group). Listening to the stories of other women helped me better understand the real side effects – not just the one or two ones that the doctors inform you about.
When patients are doing surgeries that involve immediate reconstruction, they are usually still mentally coping with having been told you have cancer. In some cases you only have a week or two (or less) to make a decision about the type of surgery you want. You are overwhelmed with information about cancer itself, and yet need to decide what surgical options are best for you. It is overwhelming at best.
I’ve helped a few women through their early journeys in treatment. I have given ‘the talk’ a few times. The talk that I give is about how breast cancer metastasizes and what you really need to look for / worry about. I find that doctors don’t give enough detail. They tell you that you are now cancer free (in remission) and only give you a vague idea of what symptoms you should be looking for. After that, every ache or pain scares you. I should know, I’ve gone through many scares. So now I help educate women about what it looks like and what warrants worry and what doesn’t. But I also need to wait until they are ready. When you are making chemotherapy or surgery decisions you are not ready to hear about the next steps. You are still dealing with the now. But there comes a time when you need more information–a time when you need to know more about the longer term impacts of the disease you are living with. I know when the time is right because I develop a relationship with these women. I know when they are struggling with anxiety largely because they lack information rather than the anxiety related to dealing with diagnosis (it looks different). It is when that anxiety shifts from the present to the future, that is when I give ‘the talk’.
The surgeon asks a good question. When is it appropriate to bring up the different possible side effects? When would you like to know? And my question is, when are you ready for ‘the talk’?
Feature image public domain via Pixabay.
-
Confirmation of incidental findings and foot surgery
A quick update on my incidental findings post the other day. The contrast MRI showed that the areas are indeed cysts and it is likely that they have been there all my life. They have nothing to do with the symptoms. Mostly I’m told that I need to exercise (which I do) and treat the symptoms (back pain). The good news is that it is not cancer, but also it is not something that needs me to see a neurosurgeon. The next treatment, if I feel the need for something more is an epidural steroid injection. This cannot be done until my foot heals – so no decisions for me to make until after I’m back on my feet again.
The sense of relief hasn’t waved over me yet. I was worried. I was worried about it being cancer, but I was also worried about it not being cancer. I was seeing outcomes that looked like a lifetime of pain. It didn’t sound good either way. So I’m relieved that it is neither at this point. I just wish these scares would stop. I really could use a period of time where I had no new worrisome symptoms.
Last Tuesday I had a minor toe surgery. I had put it off a couple of times. My podiatrist’s medical assistant had scared me a bit about the recovery. The doctor was a lot more causal about it. I didn’t like the inconsistency. But, alas, the pain in my foot got so bad that I had to do something. I could not put it off any longer. So, it turns out that I didn’t have as much damage to the cartilage in my toe as we feared. I did have something solid floating in the joint, which was unexpected and didn’t show on scans. This is likely what was causing most of the pain and swelling. So, it was been removed. The good news about that is that it is something that is likely not going to return. It means the surgery may actually fix the toe for the foreseeable future (rather than 7-10 years). After 20 years of pain in that toe, I have some hope that it will finally be relieved.
For the next week I’ll mostly be sitting on the couch or in front of my computer. Elevating the foot, teaching, or working on my dissertation. Exercise is on hold until the foot is better. Stitches come out in two weeks and we start with getting the joint moving again. I’m hoping to be hiking again within a month. Things are looking good again. And now, I feel the need for a nap. The stress of the last month is catching up to me. The back pain, the toe surgery, and my father’s passing has been a lot all at once. I could sleep for a week.
Feature Image by krozak@ CC 2.0 license.
-
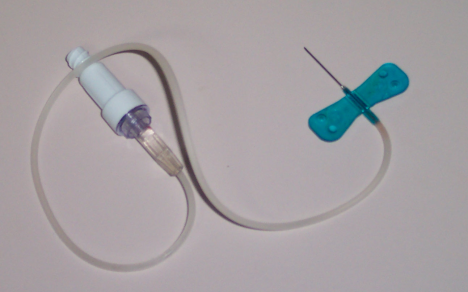
A stick in the foot
I follow the nurse into the infusion treatment area (ITA). There is a familiarity to it, and yet it is new to me. I reflect on how nice this ITA is. This is the ITA that I chose not to use when I did my treatment. Not because of the niceness. I knew that the ITA was nicer here than where I got my treatment, but I like the doctors better.
The nurse seats me in the brand new infusion chair. As with all my treatments, I was chipper and smiled while the nurse setup to jab me. I figure that they have enough grumpy people in the ITA that I do not need to add to that burden.
I remove my shoes and socks. The nurse uses the electronic function of the chair to raise my feet, which also lower my back into a semi-resting position. I feel like I’m relaxing in a recline, ready to take a nap except that my feet are cold. She puts a warming pad on my right foot in hopes to make the veins easier to find.
She puts on the blue gloves, unpacks the blue butterfly needle, and prepares to jab me. I close my eyes and then pain. Ouch. ^&%$. She moves the needle around, and with each move I’m subjected to another bout of sharp pain. Ouch. Then no blood. She removes the needle and prepares to try again. I comment that the needle seems really big/thick. She tells me that the MRI folks require the thicker needle. This time she uses a pink butterfly needle. It is like my veins are playing ‘hide-and-go-seek’. They do not want to be found. She finds a new spot in my foot. I close my eyes again. Again I feel the sharp pain as she tries to find a vein. Again she fails. Again she moves the needle around. Ouch. No luck this time.
They have a rule at that ITA. The nurses only get two chances to stick you. If they don’t have any luck then they have to find another nurse to try. The new nurse comes and we again put the warming pad on my foot. She identifies a new vein in my foot. I close my eyes. This time the stick is not nearly as painful. The nurses realize that by raising my foot they are not getting blood flow. Once the needle is in, they lower my feet. Blood trickles out of the needle. Yay. I don’t think I could handle a fourth stab.
The nurse crouches over my foot IV filling the vial with blood. When the vial is full she prepares the saline flush. I recall that I will be hit with a taste and smell of saline that comes from inside my body. I associate that taste with the access of my port for chemotherapy treatments. It is a familiar feeling. What is interesting is that the reaction is delayed. With the port, the taste-smell of saline happens immediately. In the foot it takes about 10 seconds before I get that taste-smell sensation.
With an IV in my foot I cannot walk the distance required to get to the MRI. The nurse finds me a wheelchair and delivers me across the medical campus to the MRI imaging center.
You might be asking why I’m getting an IV in my foot? Since my bout with minor lymphedema last year, I’m not allowed to get IVs in my arms. The cancer surgery involved the removal of a few lymph nodes from each arm. Since I’ve already had a minor (very minor) bout of lymphedema in my left arm, my lymphedema doctor has proclaimed that I should not get IVs in my arms. Fortunately I can still do blood draws on my right side, so I do not need to go through this production of getting a foot IV that often.
I am learning that I will forever be familiar with the local ITA. The ITA is where the nurses are at can do things like access veins in my foot (which often requires doctor approval). I find that interesting too. I’m the patient. I’m the one telling the schedulers and nurses that I need the IV in my foot rather than my arm, and yet they sometimes need to call a doctor to get approval for it. Fortunately, the nurses in the ITA get it. They understand what it means to have lymph nodes out on both sides. They see it. Maybe not every day, but often enough to know.
I see my lymphedema doctor at the end of October for an annual follow up. Since I no longer have any symptoms (no swelling in my arms), I’m hoping that I can relax the precautions a little. It is a difficult choice. I’m at a lifetime risk of getting lymphedema. My risk was considered really low, and yet it happened. So now, I wonder, how careful do I need to be? Especially when that careful involves added pain? This is yet another quality-of-life question.
Feature image Public Domain: https://en.wikipedia.org/wiki/Winged_infusion_set#/media/File:Butterfly_needle.png

