Originally mom was told there were no clinical trials that she qualified for. Kidney cancer is rare, and papillary renal cell carcinoma (pRCC) is a rare form of kidney cancer. Fortunately, she was informed that there was a clinical trial that she qualified for (or will qualify for after treating her brain mets). pRCC is an aggressive form of RCC.
The trial is known as the PAPMET trial, and it is looking at the effectiveness of MET Kinase Inhibitors in pRCC. Currently, the treatments they use to slow the progression of pRCC are the same treatments as RCC – that is, they don’t have any treatments that are specific to pRCC and as such, it is unclear whether or not the treatments are effective. The PAPMET trial compares the standard of care, Sutant, with three MET Kinase inhibitors (Cabozantinib, Crizotinib, Savolitinib). The drugs have slightly different names in the US trial but I think that is the use of generic names versus brand names. In either case, the papmet trial is the same trial in Canada and the US. I found the Canadian trial website that has a lot of great information about the trial.
As of March, the trial which started in April 2016 has enrolled 72 patients in the US and 5 in Canada. The full trial needs 180 patients. It follows patients for 3 years, and is expected that two years after the last patient has completed the trial (so five years after the last patient begins) the trial will have complete results. It is a phase 2 trial.
I read through a bunch of the information on the website, and looked at exclusion criteria. The only one that is of concern is:
“Patients with a history of treated brain metastases who are asymptomatic and have not received steroid therapy in the 14 days prior to registration are eligible. Antiseizure medications are allowed provided they are non-enzyme inducing (e.g. topiramate, levatiracetam, gabapentin).” (Protocol document, p. 39).
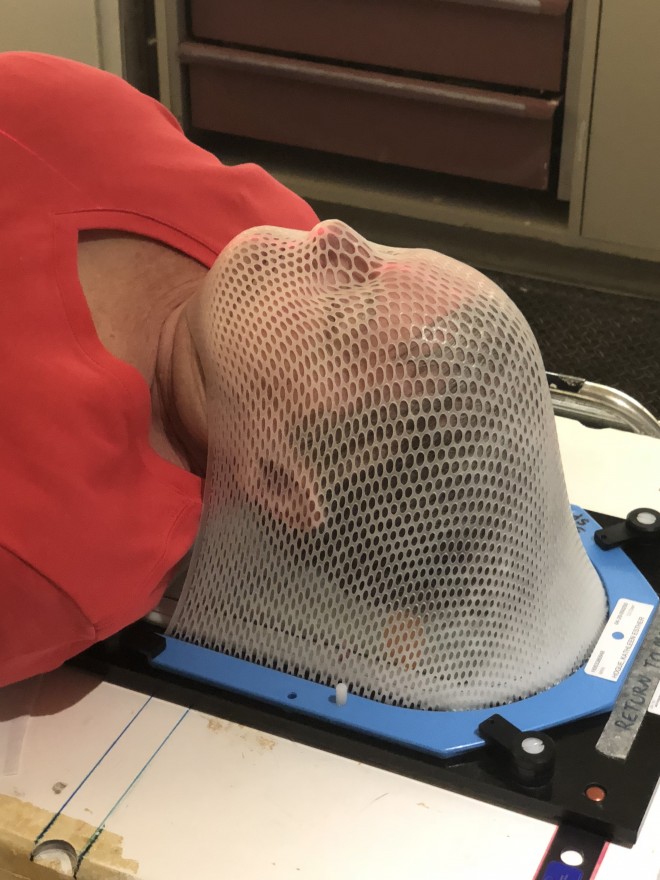
The way people have explained brain mets to me, is that you get one doctor that treats you from the head up (the neuro-oncologist) and the other (medical oncologist) that treats you from the head down. I am expecting that the neuro-oncologist will recommend some form of stereotactic radiotherapy (Cyberknife is a particular brand of stereotactic radiotherapy – I’m not sure what kind is available at mom’s local clinic). In a previous post, my friend Dawn explains her experience with Cyberknife. With brain tumours, they typically do the treatment and then watch and wait – that is, they do a follow up scan in 3-months unless there are new symptoms which prompt a faster scan. Note that this is not brain cancer, rather it is kidney cancer that has spread to the brain. Mom is doing a brain MRI today and will see the neuro-oncologist on Monday. I hope that they can get this treatment planned so that it happens either before I get back there or while I’m there.
The PAPMET trial focuses on the head down. Mom needs to get the brain mets treated first, and then once that treatment is complete, 14 days later, she can begin the PAPMET trial to start slowing the growth of the tumours from the head down.
Once she is in the trial, they do scans every 42 days (that is, after each cycle of the medication) to see whether or not the tumours are growing. They are looking for progression – that is tumour growth. They are comparing the different medications to see which one provides the longest progression free survival (PFS), but also measuring drug toxicity and quality of life. There is little point in taking a drug that makes your life suck, even if it slows the growth of the cancer.
It is a bit frustrating, the feeling of waiting and knowing that the cancer is going untreated while we scan and wait. I’m also conflicted about my plans. I currently have plans to go to Canada on May 20th, but I don’t have a return date set – however, I do have a retreat / kayaking trip planned for June 9-10, so my plan is to definitely be back in California by then. I’m conflicted about my needs for self-care. I’m torn between being in two places at once, about not being here for my friends that need me, but also not being at home with mom when she needs me. And then there is the guilt of needing to not put my own life on hold – the need for my husband and I to take a vacation because we cannot keep going without taking a break. We need to recharge, but the way we recharge usually involves being completely off-grid – away from contact – which means no way to reach us for days at a time, and that too is a challenge when things can change so very quickly.
For now, I’m providing remote support. I’m making lists of questions for the various doctors. I’m trying to get information to help better understand the options and what is happening. That is something I can do. I’m also doing some physical stuff. I’m sanding and finishing the cabinets for the van. I’m working on the weed infestation behind the house – putting down new landscape fabric and rocks in the hopes of keeping the larger 3-4 foot weeds out and allowing some native ground cover to grow – right now the ground cover had pretty orange flowers. I’m playing in my garden, and whenever I have the chance, I’m getting out for a hike.